
The Weill Cornell Primary Care program is a targeted 36-month residency that provides a focused outpatient medicine curriculum in addition to intensive inpatient training. Established in 1989, it is characterized by its clinical rigor and flexible opportunities for academic exploration. There is an emphasis on the development of excellence in the clinical endeavor, teaching, leadership, and scholarly pursuit. It is an institutional priority that residents learn how to think about health care disparities, health equity, delivery of care, community outreach, and evidence-based care, topics particularly relevant in medicine and in our society.
Primary Care residents rotate through the same inpatient clinical rotations as Categorical residents – including general medicine, subspecialty medicine, and intensive care rotations – but have additional dedicated time devoted to primary care medicine, including spending a full six months of both the PGY2 year and the PGY3 year training in the ambulatory setting. This enriched ambulatory time is devoted to direct patient care in the resident's continuity clinics, ambulatory subspecialty electives with expanded didactic and clinical exposures, regular evidence-based medicine journal clubs, a mentored longitudinal scholarly project, a unique PGY3 leadership/teaching role as Assistant Ambulatory Chief Resident, and attendance at annual Society for General Internal Medicine meetings. All of these exposures prepare residents in the Primary Care track to become consummate academic general internists, to care for adult patients across the spectrum of internal medicine, and to assume leadership roles in their careers.
Increasing the number of primary care trainees and practitioners represents a critical contribution to addressing the current health care crisis on many fronts, including access, value, and quality of care. Primary care physicians are generalists trained in the entire breadth of internal medicine, both chronic and acute. They build longitudinal patient relationships, offer comprehensive patient-centered care, and improve access to care and health outcomes for their patients. They are leaders in clinical medicine, academic medical education, community outreach, and patient advocacy. We are proud to contribute to this valuable tradition and to train the primary care leaders of tomorrow. Join us!
While the Cornell Primary Care track is fully integrated into the larger Categorical Residency program, it has special characteristics that set it apart. Note, it has a separate match through its unique NRMP program number.

The program offers diverse clinical practice opportunities including:
In addition, it offers a range of academic exposures including:
Above all, the program affords a great degree of personalization and flexibility which allows residents and program leadership to work together to tailor a training experience specific to the individual's needs and interests. Residents both develop excellence in an area of clinical practice but also explore areas of interest within the scope of academic general internal medicine, including clinical research, medical education, medical ethics, public health, and health policy. Graduates of the program are well poised for careers as general internists, clinician-educators, clinician-investigators, and patient advocates.
Primary Care residents rotate through the same inpatient clinical rotations as Categorical residents, but have additional dedicated time devoted to outpatient primary care internal medicine during the PGY2 and PGY3 years. The breakdown is as follows:
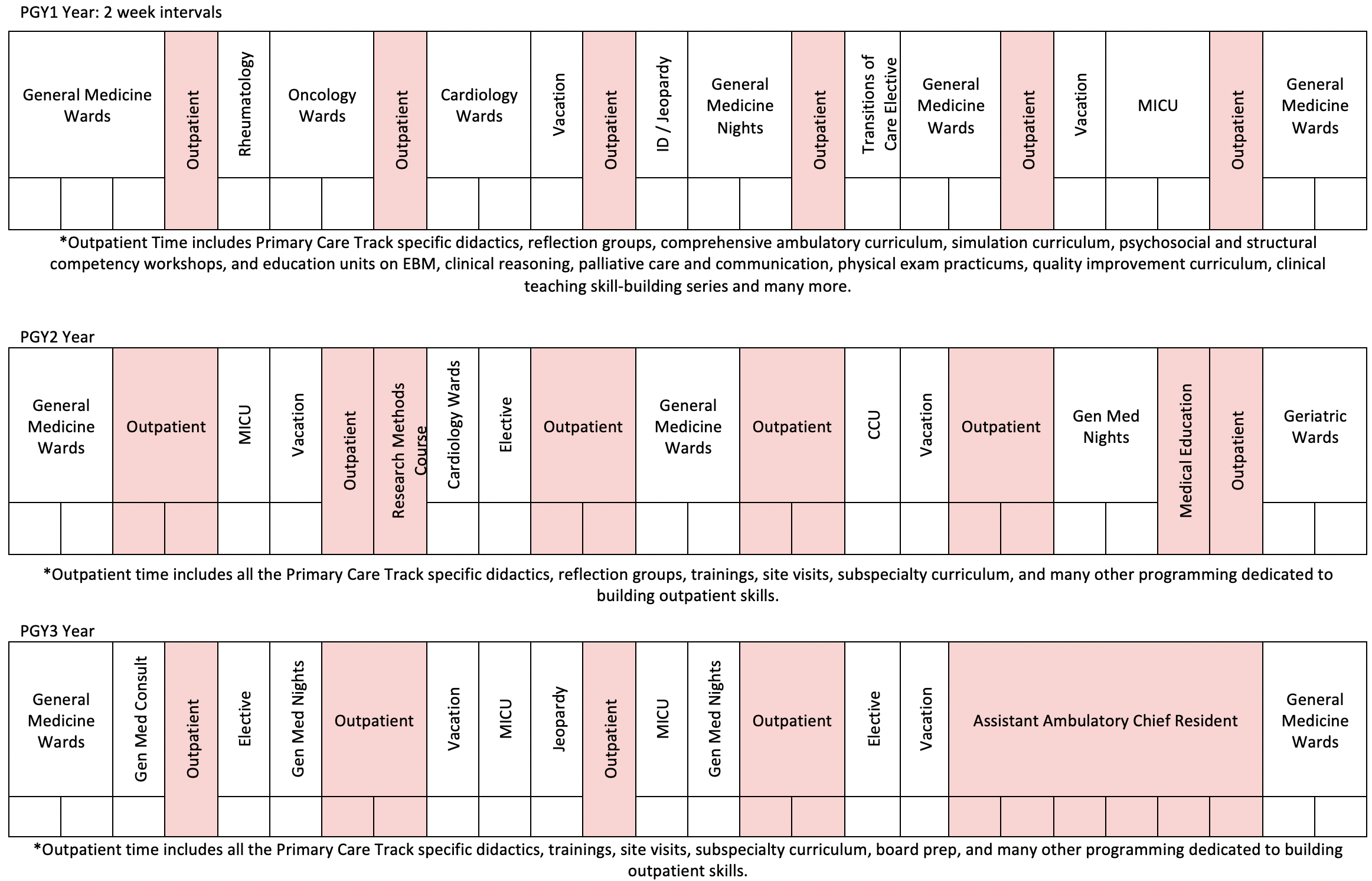
Schedule is at two-week intervals
PGY1: Outpatient Time includes Primary Care Track specific didactics, comprehensive ambulatory curriculum, simulation curriculum, psychosocial and structural competency workshops and education units on EBM, clinical reasoning, palliative care and communication, physical exam practicums, quality improvement curriculum clinical teaching skill-building series and many more.
PGY2: Outpatient Time includes all the Primary Care Tract specific didactics, trainings, site visits, subspeciality curriculum and many other programming dedicated to building outpatient skills.
PGY3: Outpatient Time includes all the Primary Care Track specific didactics, trainings site visits, subspecialty curriculum, board prep, and many other programming dedicated to building outpatient skills.

Residents practice side-by-side with faculty at one of three fully integrated outpatient practice sites, providing comprehensive care to a truly diverse patient population. Both residents and faculty see a broad payer-mix, including privately insured, Medicare, and Medicaid patients in approximately equal proportions. The patient population is multi-cultural and multi-lingual, reflecting New York City's population. Residents serve as true primary care physicians for all aspects of a patient's care and become proficient in the essential components of ambulatory medicine including chronic care, urgent care, telehealth medicine, prevention and screening, and patient education. In the context of the current public health crisis, residents are trained in best-practices for video-visits and tele-medicine platforms.

In the second half of residency, Primary Care residents participate in a second weekly continuity clinic outside of their main practice site. The second continuity experience allows residents to build a longitudinal relationship with a patient panel, honing specific clinical skills in a focused area of primary care.
Sites vary widely and have included HIV medicine, Endocrine, Gynecology, Nephrology, Rehabilitation Medicine, Adolescent Medicine, Weight Management, Psychiatry, Medical Genetics, Rheumatology, Neurology Memory Clinic, Home Visits, and work with the New York City Department of Health. Selections are driven entirely by our residents' interests.

All Primary Care residents serve as the Assistant Ambulatory Chief Resident (ACR) during 2-3 months of their senior year, an experience unique to our program which provides a wonderful opportunity to act as a clinical educator in the practice. ACRs assume a leadership role and refine their teaching skills by taking responsibility for presenting morning reports two days per week for all residents on their ambulatory rotation. To prepare our residents for this medical educator role, all primary care residents additionally participate in the medical education elective in their PGY2 year. In this course, residents learn hands-on practical teaching skills while improving their ability to analyze teaching and promote understanding and retention in learners. Sample topics include: learning climate, education theories, evaluation and feedback, putting together talks, building educator portfolios, identifying learners in need, and education research.
Additional responsibilities of the ACR include supervised precepting of Housestaff, assisting with administration for the Primary Care program, and an important role as the liaison between residents and faculty at the WCIMA practice site. This valuable opportunity mirrors the responsibilities of junior academic faculty and teaches trainees about managing an outpatient practice, clinical administration, teaching, and leadership skills.

All primary care residents participate in a structured research course as preparation for their required scholarly project. Both didactic lectures and small group mentoring sessions to discuss residents' projects in detail are specifically designed to direct the efforts towards a published end-product. Primary care residents during PGY2 and PGY3 year have additional protected time dedicated to independent work on their project. They present regular updates to their peers and to the Primary Care core faculty for feedback, support, and mentorship. Whether it is a resident's first foray into scholarly work or they already have advanced research skills gained through an MPH or other degree, the Primary Care research curriculum is designed to be flexible enough to meet each individual trainee's needs and help them reach the next level of scholarly achievement.
Our residents have produced some impressive work, most presenting their abstracts at national conferences and some going on to careers as clinician-investigators. Prior projects are diverse and have included the design and evaluation of a curriculum on PrEP, the interrogation of a large clinical database to elucidate the relationship between caregiver burden and health, the development of peer-reviewed patient education materials for an online medical resource, a systematic review of social media in resident education, a chart-review evaluation of outcomes in an obesity management clinic, a qualitative exploration of what drives physician social engagement, and an assessment of post-hospitalization mortality in Tanzania, among many others. Please review selected examples of recent resident publications.
The Primary Care subspecialty curriculum is organized around clinical themes including dermatology, cardiopulmonary medicine, musculoskeletal medicine, women's health, endocrinology, psychiatry, and neurology. A combination of rotations in specialty clinics, syllabus readings, and case-based conferences serve to concentrate the learning experience around management of common outpatient and subspecialty conditions. At a resident's initiation, time can also be set aside for individual specialty electives of the resident's choice.
The Primary Care Health Equity Reflection Series is organized around themes related to health equity and social determinants of health, including housing insecurity, food insecurity, incarceration, reproductive justice/gender health, disability in medicine, addiction medicine, mental health and racism, immigrant health, and other professional development topics. To build awareness and find moments for advocacy, this series includes site visits, journal clubs, and guest speakers from community leaders and the diverse community based organizations of New York City. Additionally, second and third year residents receive didactics on Medication-Assisted Treatment as they rotate through our Medication-Assisted Treatment clinic embedded in our primary care clinic at WCIMA Helmsley Medical Tower.

Once weekly during ambulatory blocks, Primary Care residents and faculty meet together and discuss evidence-based "answers" to clinically relevant questions formulated during the previous week of practice. Two residents are chosen to identify a focused clinical question, demonstrate their literature search strategy, and summarize the relevant article(s). By keeping these searches focused and succinct, residents develop the skills necessary to incorporate evidence-based searches into their standard practice, including formulating an answerable clinical question, searching the appropriate databases, appraising the literature critically, and applying the results to patient care.
An extensive ambulatory curriculum is delivered in a morning lecture series to ensure all residents graduate with a solid foundation in general medicine. Topics include hypertension, diabetes, musculoskeletal complaints, asthma, COPD, thyroid disease, cardiac testing, GERD, mental health, pain management, women's health, travel medicine, and age-specific screening, sexual health, LGBT health, to name just a few. In addition to the ambulatory lectures, time is dedicated two mornings a week to Morning Report presentation of outpatient cases, led by the Ambulatory Chief Resident. Generalist faculty attend to enhance the discussions.
Primary Care PGY3 residents are offered the same opportunities to participate in global health electives as Categorical residents, including structured rotations at sites in Tanzania, Haiti and Brazil. Please see What Sets Us Apart: Global Health Offerings for details. In addition, the Primary Care track offers PGY2 residents valuable flexibility to structure some of their elective time for international clinical and/or research electives.
All PGY2 and PGY3 Primary Care residents are invited to attend the national meeting of the Society of General Internal Medicine (SGIM) each spring, provided the resident submits an abstract or clinical vignette to the conference. The SGIM conference is an incredible meeting of leaders in academic general medicine and represents a great opportunity for residents to learn about the national agenda for general internal medicine. Residents are encouraged to get involved in the wide range of activities offered through the society and to use the meeting time to develop ideas for their own projects, explore career options, make contacts, and learn about primary care internal medicine. Primary Care PGY1s are invited to attend the regional SGIM meeting. This year, the meeting will be held virtually, so we will join together in a socially distant setting to participate together.
Learn more about SGIM and view the division of General Internal Medicine's ![]() 2024 program booklet.
2024 program booklet.
The Primary Care residents enjoy good eating and casual socializing as often as possible! The Assistant Ambulatory Chief Resident organizes a group get-together about once every two months to foster camaraderie amongst the Primary Care classes. Other, more formal gatherings include the Intern Welcome Party, Alumni Networking and Career Night, and the Senior Graduation Party. Our Primary Care residents are strongly bonded, lending each other support, friendship, and strength.