About Us

At the heart of our mission is a deep commitment to delivering exceptional inpatient care—rooted in clinical excellence, collaboration, continuous learning and innovation. We strive to provide equitable, compassionate and patient-centered care to every individual, every day.
Our distinguished team of approximately 100 academic faculty members provides expert inpatient care across two premier campuses— NewYork-Presbyterian Weill Cornell Medical Center and NewYork-Presbyterian Lower Manhattan Hospital.
Together, we care for approximately 350 inpatients daily, leading general medicine inpatient teams with internal medicine residents and physician assistants and working as consultants on general medicine consult and surgical co-management teams.
Beyond clinical care, our hospitalists are pioneers in medical education, healthcare quality and research. Many have pursued advanced degrees, including:
Master of Public Health (MPH)
Master of Science (MSc)
Master of Health Professions Education (MHPE)
Doctor of Philosophy (PhD) in Sociology & Health Professions Education
We take pride in shaping the future of medicine, serving as course directors and mentors in undergraduate and graduate medical education, as well as holding key institutional leadership roles. Our faculty’s research contributions are widely recognized, with multiple NIH K and R01 awards, foundation grants and over 659 publications since 1996.
At the forefront of innovation, education and compassionate care, we are dedicated to making a lasting impact on our patients, our trainees and the field of medicine.
Hospital Medicine Leadership

Chief of Hospital Medicine
Associate Chief of Hospital Medicine

Assistant Chief of Hospital Medicine

Assistant Chief of Hospital Medicine
Assistant Chief for Education of Hospital Medicine
Site Director at Lower Manhattan Hospital
Assistant Chief of Hospital Medicine

Assistant Site Director at Lower Manhattan Hospital
Hospital Medicine Faculty
Our hospitalists are internal medicine physicians dedicated to treating acutely ill patients in the hospital setting. Many of our faculty have pursued advanced fellowship training in specialties such as infectious diseases, nephrology, addiction medicine, geriatrics and palliative care and medical ethics. Additionally, several of our faculty have served as chief residents, reflecting their leadership and expertise in academic medicine.
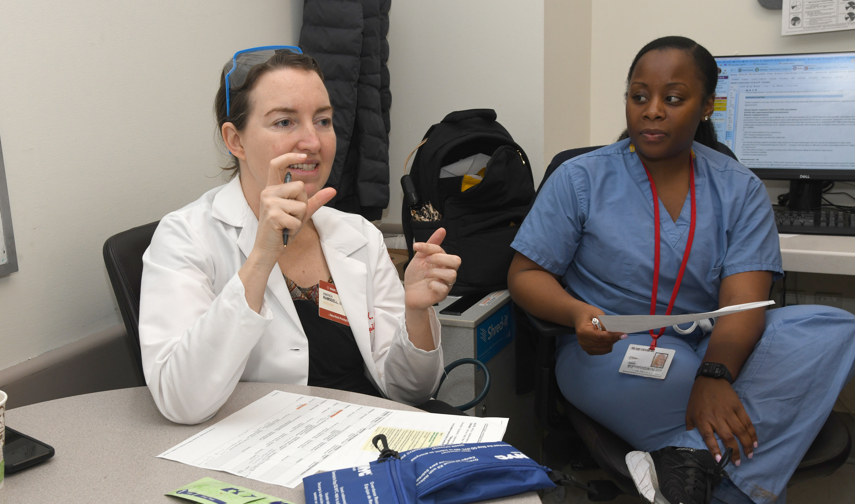
Clinical Care
Clinical care services at the NewYork-Presbyterian Weill Cornell Medical Center.
Clinical care services at the NewYork-Presbyterian Lower Manhattan Hospital.

The majority of our service is comprised of patients on the general medicine service, where we either supervise internal medicine residents or collaborate with physician assistants (PAs). Our night hospitalists work with PAs caring for patients admitted to the General Medicine and Leukemia, Lymphoma and Bone Marrow Transplant services. We consult and co-manage patients on the Medical Orthopedics Co-Management service at Weill Cornell Medicine, the Surgical Co-Management service at Lower Manhattan, and medical consultation for behavioral health inpatients at the Westchester Behavioral Health Center. Our hospitalists run a Diagnostic Point of Care Ultrasound (POCUS) with Bedside Procedure service and addiction medicine consult service. Our hospitalists also work on the clinical ethics consult service.
Career Opportunities
We are recruiting academic hospitalists—those just finishing residency or fellowship, as well as mid-career and senior hospitalists— for both full-time or part-time positions. Traditionally, our recruitment season begins in the late summer and early fall of each academic year (August/September). Detailed information about our program, expectations, along with specifics on the application process is available here.
We expect our academic hospitalist faculty to not only provide exceptional patient care but engage in leadership and scholarship in their areas of interests spanning medical education, quality improvement, research, informatics, ethics, addiction medicine, health equity, health services, among other topics. We pride ourselves on faculty members’ robust participation in Hospital Medicine’s culture of collegial support and professionalism.
We invite you to explore our open faculty positions.
We offer the following faculty development and training programs:
Clinical Scholars Program

Dr. Arthur Evans
Co-Director

Dr. Alice Tang
Co-Director
Clinical Scholars Program (CSP) is a one-year professional development program for early career faculty, to develop essential academic skills and jumpstart a successful career as an academic hospitalist. This program provides intensive mentorship and skills training in medical education, bedside teaching, POCUS, medical ethics, quality improvement methodology, evidence-based decision making and leadership. It also provides academic mentorship for development of scholarship. Please see a detailed description available here.
POCUS Fellowship

Dr. Tanping Wong
Fellowship Director
Point of Care Ultrasound (POCUS) Fellowship is a one-year program to gain expertise in diagnostic POCUS, ultrasound-guided bedside procedures, teaching and program management. Approximately 50% of time spent as hospitalist attending and 50% spent as a fellow for POCUS training and mentorship of academic project. The goal is to prepare for a POCUS-related leadership role in academic medical centers. Please see more information and a link to the application available here.
Addiction Medicine Fellowship

Dr. Amanda Ramsdell
Fellowship Director
Addiction Medicine Fellowship is a one-year program, usually spread over two years, with approximately 50% of time spent as hospitalist attending and 50% in fellowship training (in partnership with Department of Psychiatry), with the goal to join a successful group of our faculty who combine a career in hospital medicine with inpatient consultation and outpatient addiction medicine clinical care. The fellowship is most appropriate for faculty with a few years of experience as an academic hospitalist.
Hospital Medicine Medical Ethics

Dr. Nekee Pandya

Dr. Ezra Gabbay
The Hospital Medicine Section faculty has longstanding, robust collaboration with the Weill Cornell Medicine Division of Medical Ethics. Several hospital medicine faculty have trained and served as clinical ethics consultants, drawing upon their unique perspectives on clinical care, medical education and the psycho-social determinants of health. Hospital medicine faculty also serve as site directors for Ethics at NYP- Lower Manhattan and Brooklyn Methodist Hospital.
Hospitalists at Weill Cornell Medicine are also involved in ethics education, serving as faculty in several ethics courses including the Essential Principles of Medicine, Health, Illness and Disease and Advanced Clinical Ethics courses.
The collaboration between hospital medicine and ethics has produced an extraordinary body of scholarship, with peer reviewed publicationsencompassing clinical ethics, medical humanities, religion and medicine, history of medicine and other disciplines.
Simulation in Medical Education
The Weill Cornell Medicine NewYork-Presbyterian Simulation Center’s Fellowship in Simulation Education offers healthcare professionals an exciting opportunity to become leaders in interprofessional and interdisciplinary simulation education through experiential learning. Fellows will work with experts in medical education to develop simulation curricula, design research projects, become proficient in simulation operations and learn to manage a simulation program. To learn more, please see here.
Research Fellowships
 Dr. Monika Safford
Dr. Monika SaffordCo-Director

Dr. Margaret McNairy
Co-Director
The Division of General Internal Medicine provides hospitalists with multiple opportunities for research mentorship and training. Our two most common pathways are the Cornell Hunter Health Equity Research Fellowship and the Cornell Global Health Research Fellowship. Each fellowship is two to three year post-doctoral training for researchers in primary care, inpatient care and global health designed for physicians to become independently research funded. Themes of the fellowship are research in health services, health equity and global health. Typically, physicians spend around 20% with clinical time 80% research.
Additional Faculty Development Programs
The following training programs are to be expert coaches or expert group peer mentors. The programs are available to faculty with at least two years of experience.
- Master Coach Program is a one-year faculty development program aimed to train faculty as coaches, to champion growth mindset and deliberate practice in Academic Medicine through coaching. Participants hone their coaching skills through engaging with the coaching community during a longitudinal skills development curriculum and peer coaching in the clinical environment.
- Group Peer Mentoring Program is a novel faculty development strategy. It consists of small groups of 8-12 faculty and meet four times a year for full day long workshops with trained facilitators, and complete assignments with peer mentors on topics between each session. Topics include reflection on values, strengths, career vision, and legacy, design thinking, long and short-term goal-setting and planning, personal-professional integration, mentoring frameworks and skills and leadership training.
We have 15 hospitalists with extramural funding for research, with research activities that include NIH career development awards (K awards), clinical trials, epidemiologic cohorts and implementation science studies. Our faculty also lead domestic and international research training and capacity grants. Please learn more about our recent publications.
Education
Our hospitalists teach 120 medicine residents each year and serve in residency leadership roles: four hospitalists are APDs and seven other hospitalists are advisors or core faculty who lead curricula for PGY1, PGY2 and PGY3 residents. These classes include the following curricula: Compassionate Care, Quality Improvement, Evidence Based Medicine, Medical Education and POCUS. In addition, all medical residents spend at least three months on a General Medicine Inpatient Medicine team with a hospitalist attending.
Our hospitalists also lead and teach over eight faculty development or fellowship programs, such as Clinical Informatics and Quality and Patient Safety focused on advanced academic skills, POCUS, addiction medicine, medical ethics, quality improvement, simulation and research. Additionally, we have a Diversity, Equity, and Inclusion program to promote cultural diversity among the faculty, fellows, and house staff. There are 24 hospitalists who have additional advanced degrees—Masters, PhD, or MBA—and 21 (including four CMR from incoming cohort) who were chief medical residents.

