The Division of Gastroenterology & Hepatology has a wide range of active ongoing research on gastrointestinal and hepatic conditions and disorders. This research includes basic science research, translational research, clinical research studies and clinical trials. Research is a core component of the division’s mission and is focused on the areas of gastrointestinal inflammation, infections and its immune system, the gut microbiome and fecal transplantation, inflammatory bowel disease (IBD), hepatitis B and C, Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) (formerly known as fatty liver disease), liver and GI cancer treatment and prevention (including cancer genetics), advanced endoscopic procedures, pancreatic and bile duct lesions, obesity, HIV-related GI and liver diseases, as well as other gastrointestinal diseases and conditions. Numerous studies and clinical trials are underway to understand the mechanisms of these diseases and how to best prevent and treat them.
The division has a long history of clinical research in the causes, prevention, and treatment of patients with liver disease and hepatitis and is recognized as one of the leaders in the field. The Center for Liver Diseases at NewYork-Presbyterian Hospital is the largest liver transplantation program in the region and has a significant clinical research program in a wide variety of liver diseases.
The division, together with Rockefeller University and NewYork-Presbyterian Hospital, established The Center for the Study of Hepatitis C--the only comprehensive, multidisciplinary center dedicated to the study of hepatitis C and hepatic disease in the tri-state area. In addition, the division maintains a biobank for the collection and maintenance of tissue samples, used for basic science and clinical research. Other research is focused on MASLD and its link to cancer, as we seek to develop state-of-the-art systems that will provide basic understanding of liver damage and scarring, which can lead to cirrhosis.
The Jill Roberts Center for Inflammatory Bowel Disease (JRC) is an international leader in the research, diagnosis, and treatment of Crohn’s disease and ulcerative colitis. Its mission is to transform patient care through personalized therapy and progress toward a cure. Committed to “lab-to-life” research, JRC translates cutting-edge scientific discoveries into safer, more effective treatments that are reshaping the future of IBD care.
A cornerstone of this effort is the SMART IBD initiative—Stratifying Medication Response and Refractory to Therapy IBD—designed to uncover why some patients respond to treatment while others do not. By collecting longitudinal clinical data and biological specimens from every patient starting biologic or small molecule therapy, SMART IBD provides critical insights to optimize treatment strategies.
JRC also leads several other groundbreaking studies, including research on manipulating the gut microbiome to manage IBD; the FUN-CD study, which explores a novel approach to Crohn’s disease by combining antifungal therapy with IL-23-targeting biologics; and the MOMs-IBD study, focused on improving maternal health outcomes in women with IBD.
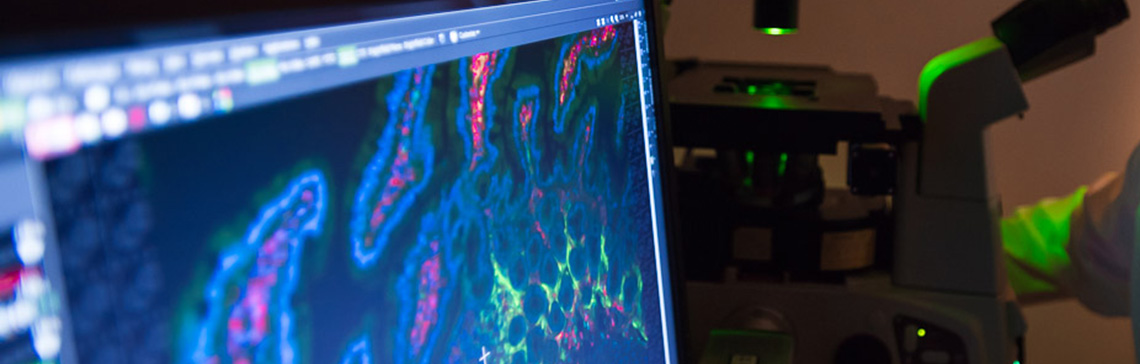
Research is conducted in partnership with the Jill Roberts Institute for Research in Inflammatory Bowel Disease (JRI) and the Friedman Center for Nutrition & Inflammation, which are both directed by Dr. David Artis. Major areas of cutting-edge research include fundamental mucosal immunology, chronic inflammation, the gut-brain axis, & the enteric nervous system in the Artis Lab and Sonnenberg Lab; the interface of diet, nutrition & the gut microbiota in shaping intestinal health, inflammation & cancer in the Arifuzzaman Lab and Collins Lab; the core mechanisms of innate immunity and phagocyte biology in the Blander Lab; gastrointestinal malignancies, genetics, and stem cell biology in the Goto Lab; the pathogenesis of IBD in the Longman Lab; and the role of the gut microbiota in mucosal immunity and cancer in the Iliev Lab and Guo Lab. Finally, through an extensive collaboration across the division and institution, we created the Jill Roberts Institute for Research in IBD WCM Live Cell Bank to rapidly accelerate clinical and translational research in gastroenterology. This biorepository is a prospective live tissue bank and database of healthy and IBD patients at Weill Cornell Medical College/NYP Hospital that collects, stores and utilizes live samples obtained from peripheral blood, gut biopsies, and fecal matter to enable functional and multi-omics studies.
Research performed by the Jay Monahan Center for Gastrointestinal Health and its collaborators is broadly focused on a multidisciplinary approach to GI cancers. Translational and clinical research includes clinicians and scientists with areas of specialization in genetics, gastroenterology and surgery. Many of our division investigators have a special interest in the causes and prevention of colorectal and other GI cancers. Projects are focused on the identification and assessment of risk factors, including determining novel genetic markers for colorectal cancer, and studies to assess if patients with a hereditary susceptibility to colorectal cancer might be able to reduce their risk by taking statins (drugs often prescribed to lower cholesterol). Laboratory studies are also being performed regarding the connection between chronic inflammation and cancer.
The Cancer Genetics program, directed by Dr. Ravi Sharaf, is leading the field of adult genetics and cancer genetics. Basic, translational and clinical research focuses on genetic testing for hereditary cancer disorders, including Lynch syndrome, familial adenomatous polyposis, hereditary pancreatic cancer, and inflammatory bowel disease. The group places particular emphasis on hereditary gastrointestinal cancer syndromes and is also working on both determining optimal screening programs as well as chemoprevention and tumor vaccines for Lynch syndrome.