Dr. Augustine M.K. Choi, the Sanford I. Weill Chair of the Weill Department of Medicine, and colleagues have published a pivotal paper in Nature Communications that has uncovered a new line of discovery regarding circadian rhythm and lung inflammation. The findings focus on the circadian-like rhythms the investigators observed in endotoxemic lungs.
As reported in their paper, entitled "Circadian Rhythm Reprogramming During Lung Inflammation," the investigators concluded that inflammation (studied in the lungs) produces a complex reorganization of cellular and molecular circadian rhythms that are relevant to early events in lung injury, and as distinct from circadian rhythms that occur in healthy lungs. This is an especially noteworthy finding when examined within the broader context of circadian rhythms, which are those daily fluctuations in biological activity that help organisms and human beings adapt to their environment. It is known that circadian rhythms have a strong genetic basis, and in recent years, a "molecular clock" located in the hypothalamus of the brain has been elucidated. This central master clock consists of "master clocks" that synchronize the oscillation of local clocks residing in peripheral organs of the body, such as the lungs. Accepting the "master clock" as a paradigm for the starting point of their study, the team also considered current theory that had assumed that these circadian rhythms are lost at the molecular level when inflammation ensues. Contrary to this assumption, Dr. Choi and colleagues asked the question: would the known circadian rhythms that regulate immune responses in animals still persist during an acute illness when the clock gene expression has been disrupted by inflammation in the organ?
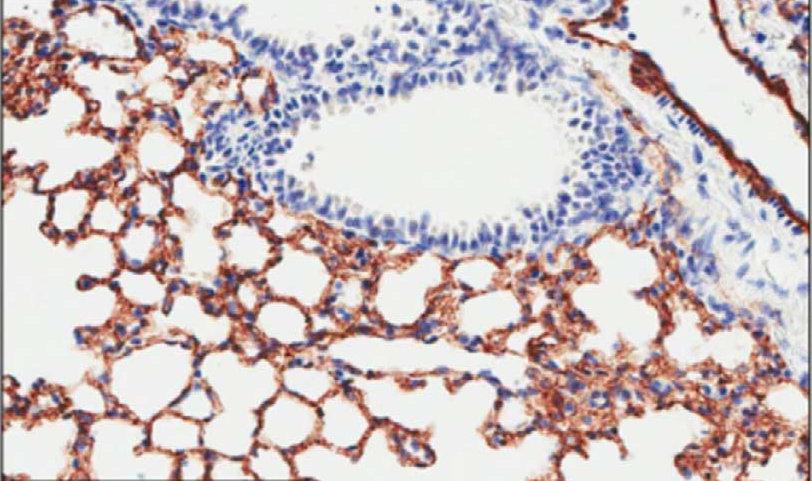
Utilizing a genome-wide approach, the investigators focused their efforts on the lungs of a mouse model subjected to endotoxemia. A world-renowned authority on lung inflammation and lung injury, Dr. Choi brought state of the art expertise to the examination of these endotoxemic lungs, with the added benefit that the lungs as an organ are an ideal setting for this type of study. The lungs represent the primary portal for systemic infection and organ failure in critically ill patients and, in this study, were shown to be a highly observable setting for the study of circadian regulation of immune processes. It is known that the circadian clocks that affect the peripheral organs influence gene expression in a tissue-specific manner. To date, there had been no data sets to establish whether or not circadian regulatory patterns occur during systemic inflammation. To fill that void, Dr. Choi and team have delivered groundbreaking data in the Nature Communications paper that is observable at the level of transcripts, metabolites, and leukocyte counts. Their results not only suggest that an alternate circadian regulatory program does emerge within the endotoxemic lung (despite disruptions to clock gene expression), it calls into question the practice of using clock gene expression patterns as surrogate markers for circadian rhythms. This practice has been applied not just to inflammation but numerous other disorders, including lung models of cigarette smoke exposure and ventilator injury.
Dr. Choi and colleagues seek to build on these advances and are now asking a new question: How are circadian-like rhythms generated in endotoxemic lungs, despite the disrupted expression patterns of multiple clock genes and disrupted metabolic feedback pathways? Answers to this and other questions will help to illuminate the circadian contributions to immunologic function during respiratory diseases and systemic inflammation.

